Some information may be outdated.
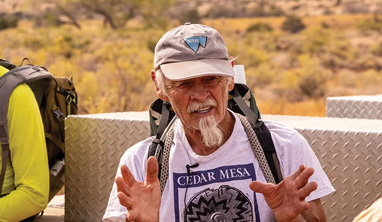
“This has been in the works since 2004,” said Grand County Emergency Medical Services Special Service District Director Andy Smith, speaking of the new, nearly-complete facility that will house the district. The facilities GCEMS has been using are inadequate and timeworn, while demands on the district have been growing. Personnel will likely move into the new building this winter.
Department grows in response to need
GCEMS transitioned from a county department to its own special service district in 2018, but long before that its leaders were looking for an appropriate facility to house the department’s equipment and personnel. Over the years, local EMS has become increasingly busy: in a report to the Grand County Commission this summer, Smith said call volume has increased 132% over the last 20 years.
Smith said the district is averaging five calls per day in 2021, and based on patterns, he expects that the district will respond to 1800 calls by the end of 2021. There were 200 calls in the month of October 2021, the most ever in a month. Even with the shut-downs caused by the pandemic, 2020 was a record year for calls for the district: In his report to the commission, Smith said EMS services were requested 1,415 times that year.
The district is funded through the healthcare sales tax and revenue from patient transports—the district provides all interfacility transports for Moab Regional Hospital, which often means driving patients from Moab to Grand Junction or Salt Lake City. Usually, around 55% to 60% of GCEMS calls serve Grand County locals; the remaining calls serve visitors or nonlocals. The district employs 47 people, 17 of whom are full-time, meaning they work two twenty-four-hour shifts and then have four days off.
The previously all-volunteer department added full-time paid positions in 2016, and the county department became its own entity in 2018. That same year, the district applied for funding for a new building from the Community Impact Board, a state body that awards loans and grants to counties and entities impacted by mineral resource development on federal lands. The CIB awarded GCEMS $1 million in grant money and $3.5 million as a zero-interest, 30-year loan. The district also contributed $120,000 of its own money into the project.
GCEMS needs space for offices, to store ambulances and other equipment, to hold trainings and conferences, and also to house staff working on overnight shifts. In the past, those needs have been met by various buildings, including the old EMS center which was built in the 1950s and demolished in November of 2020 to make way for the new building. The district has also rented space from the fire department and used county buildings. Often the district was spread between various locations, impeding quick response times and communication.
The new building
The new facility is equipped with tools and amenities that will make the district more efficient and reliable. There is a backup generator in case of power failures, and a vehicle bay that can keep all the district’s ambulances secure. The doors on the new bay, Smith noted, are two feet wider and taller than the old ambulance bay, making it easier for drivers to back in; the old “bus barn” is a tight fit for the large vehicles. Also in the ambulance bay are a secure room for narcotics used to treat patients. These must, by law, be kept in a secure location. In the old building, that was a locked cabinet; in the new facility, a cabinet kept in a separate locked closet provides added security for those substances. The bay also has a station where crews can clean and restock their gear after a call, and a balcony work-out room with weights and exercise equipment.
The old EMS center had space for the American Legion, a national nonprofit veteran’s association, and the new facility also has a meeting space for that organization. There is a training area with a dividing curtain and a large bay door to facilitate indoor/outdoor trainings. GCEMS offers First Aid and CPR courses, as well as other trainings, to its own staff but also to companies and government agencies like the National Park Service, the US Forest Service, and guide companies. Smith said the district gives hundreds of CPR certifications a year.
The new building has a “decontamination room” for when crews return from calls where they may have been exposed to bodily fluids or other hazardous materials. A washing machine and clothes dryer that meet Occupational Health and Safety Administration standards for decontamination is dedicated for use in washing soiled uniforms.
“That’ll be huge,” said Bret Sherman, an EMT for GCEMS. He remembered living with roommates and not wanting to walk into his shared home still wearing the clothes he wore while responding to a call, and not wanting to use the house laundry machines to wash clothes that may have been exposed to hazardous materials.
“It’ll be nice to not bring any of that home,” he said.
There are also a regular washer and dryer for crews to use for washing their own clothes.
“Upstairs, it’s like a regular home,” Smith said of the second floor of the new building. Crews working overnight shifts used to have the option of sleeping at their own homes, but new protocols require them to stay at the EMS crew quarters while on shift. They stay in crew quarters for 48 hours, then have four days off. The current crew quarters are in “the old white house” located next to the county offices. The house was built in the early 1900s and is roughly 800 or 900 square feet, Smith said. There are two to three beds per room and a shared kitchen while on an overnight shift. The new facility offers a newer, more comfortable and spacious place for EMTs to live while waiting to respond to emergencies.
There are seven crewmembers and two full-time ambulances on call each day. Between 7 a.m. and 7 p.m., they’re expected to be working—that might mean training, working out, resupplying bags and vehicles, or cleaning the facility. After 7 p.m., they’re on call but have the time to themselves.
A bright, open kitchen and living space offer a place to relax, read, watch movies or socialize. The kitchen has three refrigerators to help each shift keep their food items organized. Sherman said in the old crew quarters, people lost track of their condiments and bought new ones, generating dozens of bottles of mustard, for example, that crowded the shared fridge.
There are eight bedrooms, each just large enough to fit a twin bed, a closet, and a small desk. Each also has a window, fitted with blackout shades so if staff need to catch up on sleep during the day after a night on duty, they can block out sunlight. Each bedroom is also equipped with its own mini-split temperature control unit, offering occupants the best chance at getting a restful sleep in between night emergency calls. Sherman recounted “thermostat wars” with colleagues at the old crew quarters: on some shifts, staff members would wake up one by one through the night and adjust the thermostat up or down according to preferences.
Eventually, the district plans to install an alert system that only wakes up the staff who are on call to respond—that is, the crew of the ambulance that is “next up” to go to an emergency. There are, on average, Smith said, three or four calls a night—that number has been trending upward—and the current system alerts all staff who are on call that night, even if they aren’t part of the ambulance crew that will respond. Multiple sleep disturbances per night, accompanied by the elevated heart rate associated with the sense of urgency prompted by an emergency alert, can contribute to deep fatigue.
Rural EMS in distress
While it took many years for GCEMS to make the new facility a reality, its success is a contrast to emergency services in many rural areas. Smith said rural EMS centers are closing across the U.S.; news outlets have covered the challenges rural EMS providers face. A parallel trend of rural hospitals closing means that EMS is both more important to those communities, and at the same time that those providers have less support without an advanced care facility close by. A February 2021 report from the National Rural Health Association, says that over 100 rural hospitals have closed between 2010 and 2020.
Studies have identified various factors contributing to the decline of rural EMS providers.
“Rural EMS systems are more likely to be staffed by volunteers and staffed by emergency medical technicians (EMTs), and less likely to be publicly funded than their urban counterparts,” says the 2021 NRHA report. It goes on to note that volunteers often pay for their own training, which requires hundreds of hours.
Rural EMS centers cover large areas with sparse populations, meaning they have farther to drive to reach patients and thus have a smaller chance of reaching them in time to prevent injuries or emergencies from causing critical damage—at the same time, there are fewer people and fewer transports to support the base costs of readiness for rural EMS providers. GCEMS crews sometimes must travel to Green River or remote parts of Grand County, but Smith reported to the Grand County Commission that about 42% of GCEMS calls in 2020 were in Moab itself.
“Rural Americans are older and sicker than their urban counterparts, creating unique challenges for EMS providers,” reads a 2018 report from the NRHA. A high percentage of elderly people means a population at higher risk of emergencies and with more health complications; it also means fewer people are fit to be volunteer EMTs.
The 2018 NRHA report says that “Nearly one-third of rural Emergency Medical Services (EMS) are in immediate operational jeopardy.” The same organization’s 2021 policy brief recommends that legislators create funding support for paid staff in rural EMS departments.
Earlier this year, the Utah Rural EMS Directors’ Association held its annual conference in Moab. The group includes most Utah counties and about 60 EMS leaders and has a mission of unifying and empowering rural EMS directors to lead emergency medical services into the future. Smith said the gathering is a chance for EMS members to learn from each other and also to discuss legislative issues that could help support their field.
For example, a state law passed in 2020 made EMS an essential service, meaning municipalities are required to have an agreement with a provider. This offers a support system for EMS departments. The conferences also focus on helping EMS leaders learn how to effectively track data from their departments and use that data to illustrate their funding needs to policymakers.
In spite of a long history of relying on volunteers, Smith said, “EMS has never been free.”
Appreciate the coverage? Help keep local news alive.
Chip in to support the Moab Sun News.