Some information may be outdated.
“The models are not reality, but they are helpful in allowing us to know what it is that we might see,” Dr. Dylan Cole of Moab Regional Hospital said at the teleconferenced Grand County Council meeting on April 7.
> Watch the full April 7 meeting here
MRH’s chief medical officer discussed predictions of the potential spread of the coronavirus based on research and data from around the country and around the world. He emphasized that while numbers from these models can be helpful in planning for what the hospital and the community can expect, they do contain a high margin of error.
Lowering the rate of infection

Moab Regional Hospital Chief Medical Officer Dr. Dylan Cole
Cole began by discussing the average number of people that will be infected by one infected person, a figure referred to as the “R0,” (pronounced “R naught”).
Between 2.2 and 2.7 people could be infected by one person with COVID-19, most public health organizations report. Dr. Cole emphasized that this number can be lowered using effective intervention strategies like social distancing.
Dr. Cole discussed the role of asymptomatic transmission in spreading the virus. Some people may have the virus and the ability to spread it, but never experience symptoms. Others may have the virus and be spreading it before their symptoms surface.
As has been widely reported, the severity of COVID-19 symptoms has a wide range. Some estimates, Cole said, put the percentage of asymptomatic cases at 25%, with some as high as 50%.
In a case study of the Diamond Princess Cruise ship, on which virtually all passengers and crew were tested for the virus, around 20% of the ship’s population tested positive. 18% of those positives never developed symptoms, but presumably were still spreading the disease.
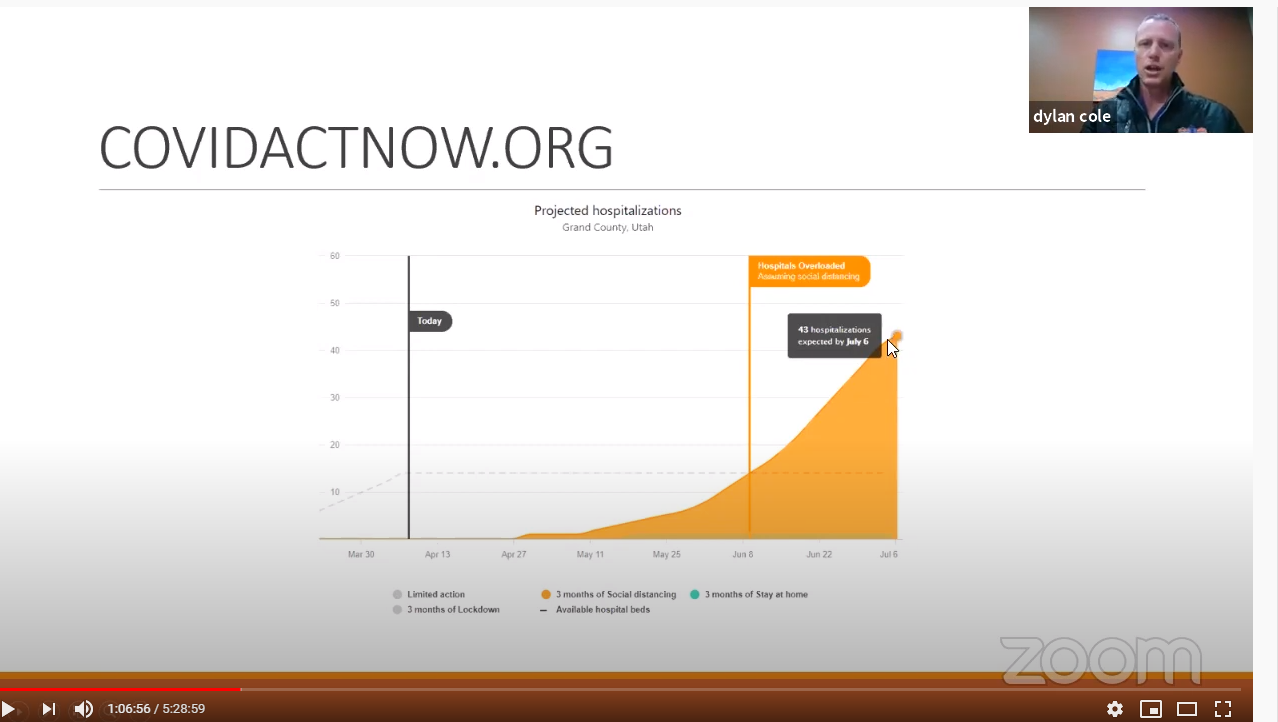
Moab Regional Hospital staff have been creating models which show how different scenarios will affect their services and Grand County as a whole.
The hospital’s service area is roughly 12,000 people in and around Grand County. Based on demographics, MRH models expect that around 10% of cases in their area will need hospital care. Of those potential cases, about a third of those needing hospitalization may require intensive care. Of those needing intensive care, 50% to 75% would require ventilators to survive. Based on rates from hospitals around the world, the hospital’s estimates show the projected fatality rate if the pandemic hits the area would be 1.5% of all those infected.
“At this point we expect, or we believe, that virtually 100% of the population is susceptible to the illness, or at least to catching it and potentially transmitting it,” Cole noted.
Using data to plan
Cole discussed a range of potential scenarios based on models from the Imperial College of London, the University of Washington Institute for Health Metrics and Evaluation, and data from case scenarios like the Lombardy region of Italy, which was hit particularly hard by the virus.
An optimistic scenario from the range of possibilities projected the peak hospital demand to be between 7-13 COVID-19 patients at one time. This scenario depends on residents practicing physical distancing to slow the disease’s spread.
In one scenario where few mitigation strategies like physical distancing are used, models show 20-30% of MRH’s service area being infected over the next 3 to 4 months. That translates to a range of 2400-3600 people.
“After a season of that spread, that would leave us with 20% of the population affected; that doesn’t mean that’s the end of the potential for further spread,” Cole clarified.
“But it does give us an idea of a modest assumption of unmitigated spread through a community in a short period of time.”
Applying the estimated averages drawn from other medical providers, that could mean from 240 to 540 people requiring hospitalization, with 72 to 180 people needing intensive care. Potential fatalities in this scenario, which is a hypothetical situation, would be between 36 and 54 people.
Cole displayed another graph that showed the spread of COVID-19 patients expected to be without mitigation strategies, models predict that the peak hospital count at 250 patients.
“With the mitigation strategies, we hope to anticipate not seeing a number like that,” said Cole.
Those mitigation strategies include social distancing and reducing travel.
Based on the different predictions about how the coronavirus pandemic could impact the area, MRH staff have created a three-level system to plan for a surge in COVID-19 cases.
In Level 1, MRH would see a peak hospital census of between 5 and 25 patients; in Level 2, a peak of between 20 and 60 patients; and in Level 3, a peak of between 60 and 150 patients.
Level 3, Cole noted, would only be expected in the absence of social distancing strategies or if “tourism were to open up again in this region all at once at full blast, we might see a surge more like that.”
Cole also noted that as more data comes in showing the effects of social distancing around the world, most models show the projected rates of spread dropping.
Questions about testing for COVID-19
Councilmember Rory Paxman asked what steps the hospital is taking now that there has been one confirmed COVID-19 case in Grand County.
“I think like many, I certainly have experienced the last couple weeks since we had that one positive [case] with a little bit of a mix of anticipation and surprise that we haven’t started to see more,” said Cole.
He said the Southeast Utah Health Department was doing the leg work on following up with the patient’s contacts.
In the meantime, the hospital is hoping to soon have expanded testing capacity and begin administering tests prioritizing populations at high risk of exposure and populations at high risk of severe infection.
“What do you need to make that happen?” asked Councilmember Evan Clapper of the increased testing capacity.
“More time,” said Cole, noting that the lack of adequate tests is not a local problem.
“The challenge in getting adequate supplies of tests and getting testing options has been problematic around the country,” he said, adding that MRH is awaiting delivery of a COVID-19 test that can give a result in 45 minutes.
County Attorney Christina Sloan asked about the nature of the tests. Currently there are two different tests discussed: “antibody tests,” which can determine whether someone has been infected with the virus and recovered; and tests that only show whether someone is sick with the virus at the time of testing.
The tests MRH hopes to have soon are called “PCR-based” (polymerase chain reaction) tests, and would only show whether a patient is currently sick. Cole said, as of now, antibody tests are more difficult to obtain.
“There is right now a disconnect between the promise that these tests are being widely distributed and the backlog” of requests, he acknowledged.
Cole ended his presentation with both hope and caution, highlighting the effectiveness of social distancing, while warning councilmembers that a flattened curve does not mean the threat is over.
“If we mitigate a peak, and we as a community are able to maintain transmission at a very low level, that’s a huge win,” Cole said. “It also creates a second set of challenges… what’s the logical way forward to prevent…a second surge? As things open back up, you still have a vast majority of the population that has not been exposed to the illness and is at a high risk of creating a second surge.”
Appreciate the coverage? Help keep local news alive.
Chip in to support the Moab Sun News.